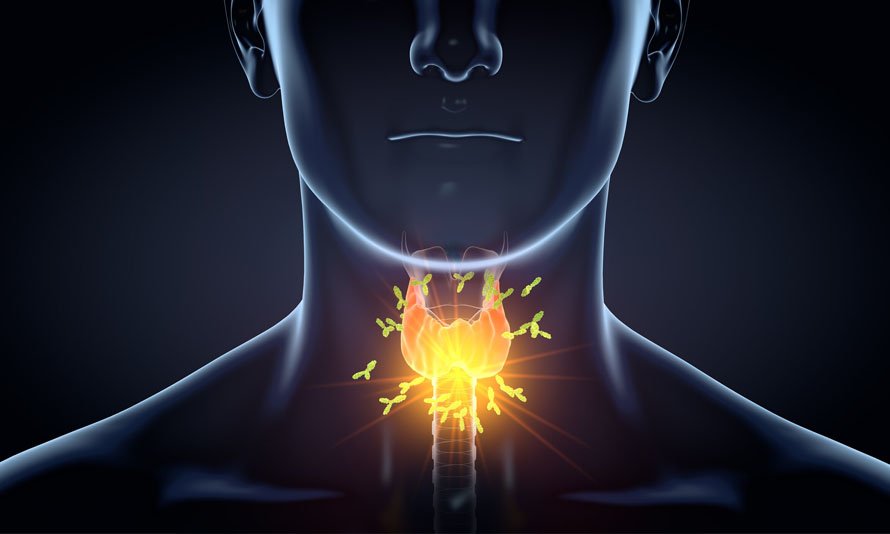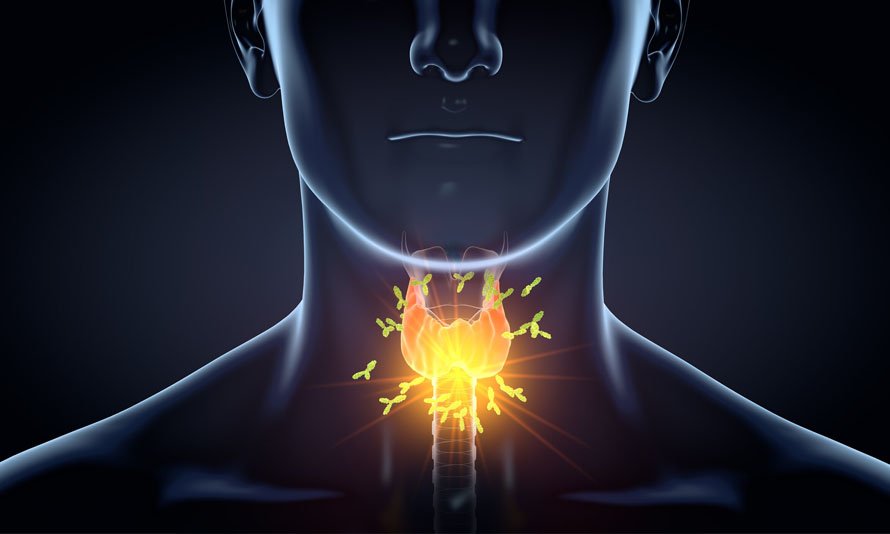
Thyroid cancer
Thyroid cancer is a relatively rare type of cancer that starts in the cells of the thyroid gland, a butterfly-shaped organ located at the base of the neck. The thyroid gland produces hormones that regulate metabolism and play a crucial role in the body's energy levels. Thyroid cancer can typically be treated successfully, especially when detected early. Here are some key points about thyroid cancer:
Types of Thyroid Cancer:
-
Papillary Thyroid Cancer: This is the most common type, accounting for about 80% of all thyroid cancers. It usually has a good prognosis and tends to grow slowly.
-
Follicular Thyroid Cancer: This type is less common and is often associated with a slightly worse prognosis than papillary thyroid cancer.
-
Medullary Thyroid Cancer: This type originates in the thyroid's C cells and may be associated with certain genetic syndromes. It tends to be more aggressive.
-
Anaplastic Thyroid Cancer: Anaplastic thyroid cancer is the rarest and most aggressive form of thyroid cancer. It tends to grow rapidly and is often challenging to treat.
Risk Factors:
- Gender: Thyroid cancer is more common in women than in men.
- Age: The risk increases with age, with most cases occurring in people between 30 and 60 years old.
- Radiation Exposure: Exposure to high levels of radiation, especially during childhood, increases the risk.
- Family History: A family history of thyroid cancer or certain hereditary conditions can elevate the risk.
- Iodine Deficiency: In areas with severe iodine deficiency, there may be an increased risk.
Symptoms:
- Many cases of thyroid cancer are asymptomatic and are often discovered during a routine physical exam or imaging for other reasons.
- When symptoms do occur, they may include a lump or nodule in the neck, hoarseness, difficulty swallowing, and swollen lymph nodes in the neck.
Diagnosis:
- Diagnosis often involves a combination of imaging tests, such as ultrasound, CT scans, and thyroid scans, as well as a fine-needle aspiration biopsy to collect a sample of thyroid tissue for examination.
Treatment:
- Treatment for thyroid cancer depends on the type, stage, and individual patient characteristics. Common treatment options include:
- Surgery: Most patients undergo thyroidectomy, which involves removing part or all of the thyroid gland.
- Radioactive Iodine (RAI) Therapy: This treatment is used after surgery to destroy any remaining thyroid tissue or cancer cells.
- Thyroid Hormone Replacement Therapy: Since surgery often removes most or all of the thyroid gland, patients need to take thyroid hormone replacement medication for life.
- External Beam Radiation Therapy: It may be used in some cases, particularly for anaplastic thyroid cancer.
- Targeted Therapy and Chemotherapy: These treatments may be considered for advanced or aggressive forms of thyroid cancer.
Prognosis:
- Thyroid cancer, especially the common papillary type, often has an excellent prognosis with a high survival rate.
- Early detection and treatment are key to successful outcomes.
- Anaplastic thyroid cancer has a much poorer prognosis and is more challenging to treat.
Thyroid cancer is typically managed by a team of healthcare professionals, including endocrinologists, surgeons, oncologists, and radiologists. Regular follow-up care is essential to monitor for any recurrence or complications. Patients are encouraged to discuss their specific diagnosis and treatment plan with their healthcare team for personalized guidance.